The healthcare industry is diverse and dynamic, offering various paths for medical professionals. Among the most popular are the Doctor of Medicine (MD) and the Doctor of Osteopathic Medicine (DO) degrees. While both MDs and DOs are fully licensed physicians who are qualified to practice medicine, there are distinct differences in their training, philosophy, and approach to patient care. Understanding these differences is crucial for patients, students, and professionals navigating the healthcare landscape.
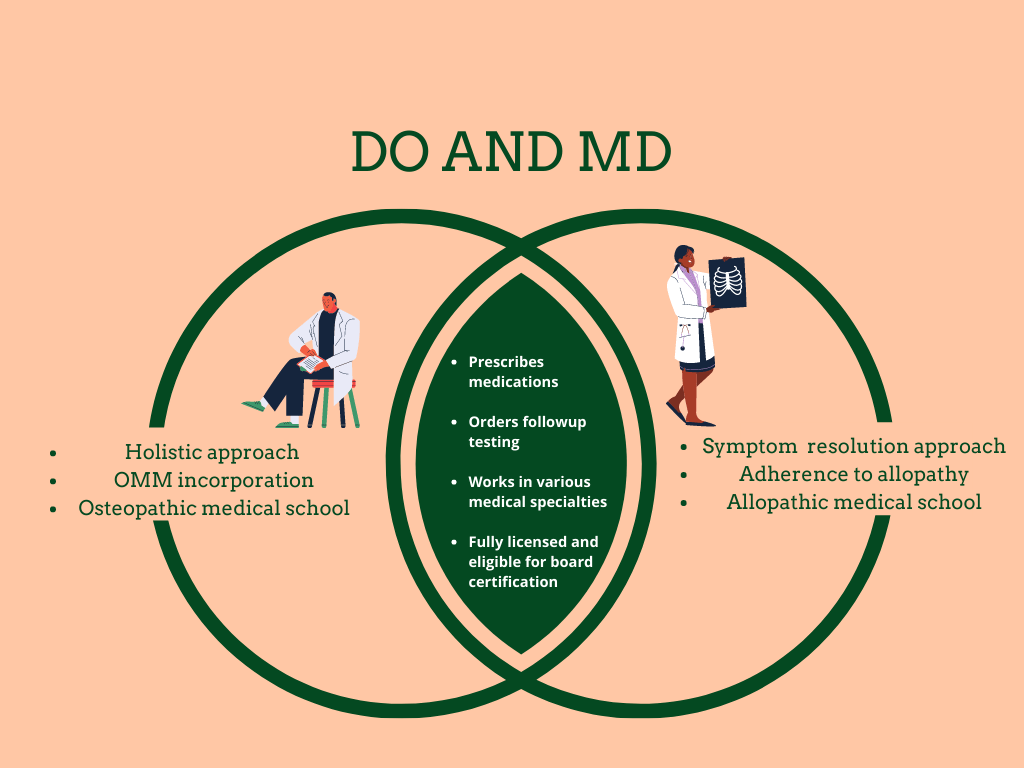
In the United States, both MD and DO degrees offer pathways to becoming a physician, yet they are rooted in different medical philosophies. MDs follow the allopathic approach, focusing on diagnosing and treating diseases primarily through medications and surgery. Conversely, DOs emphasize a holistic approach to patient care, integrating osteopathic manipulative treatment (OMT) and a focus on the musculoskeletal system in their practice. This divergence in training and focus often leads to varying methodologies in treating patients.
Choosing between an MD or DO degree can be a pivotal decision for aspiring medical professionals. This decision impacts not only the educational journey but also the career path, including residency opportunities and practice settings. By delving into the nuances of each degree, individuals can make informed choices that align with their career goals and personal beliefs about patient care. This article aims to provide a comprehensive understanding of the key differences between MD and DO degrees, offering insights into their unique characteristics and the implications for medical practice.
Table of Contents
- What is an MD?
- What is a DO?
- Historical Background of MD
- Historical Background of DO
- Educational Path for MDs
- Educational Path for DOs
- Philosophical Differences in Practice
- Clinical Approach of MDs
- Clinical Approach of DOs
- Residency and Specialization Opportunities
- Career Opportunities for MDs
- Career Opportunities for DOs
- How Do Patients Perceive MDs and DOs?
- Can MDs and DOs Integrate Practices?
- What is the Key Difference Between MD and DO?
- FAQs
- Conclusion
What is an MD?
MD stands for Doctor of Medicine, a degree conferred upon individuals who have completed medical school in an allopathic medical program. The allopathic approach to medicine involves the use of science-based practices to diagnose and treat illnesses. MDs are trained to focus on the symptoms and treatment of diseases, using methods such as medication, surgery, and other interventions.
MD programs typically last four years, with the first two years focused on classroom-based learning in subjects such as anatomy, biochemistry, pharmacology, and pathology. The final two years involve clinical rotations in various medical specialties, providing students with hands-on experience in diagnosing and treating patients.
Upon graduation, MDs must pass the United States Medical Licensing Examination (USMLE) to qualify for a medical license. They then proceed to residency programs, where they can further specialize in areas such as internal medicine, pediatrics, surgery, or psychiatry. The training and expertise gained during these years equip MDs with the skills necessary to provide high-quality medical care.
What is a DO?
DO stands for Doctor of Osteopathic Medicine, a degree that emphasizes a holistic approach to healthcare. Osteopathic medicine is grounded in the philosophy that the body is an integrated whole, capable of self-healing. DOs receive specialized training in osteopathic manipulative treatment (OMT), a hands-on technique used to diagnose, treat, and prevent illness and injury.
The educational journey for DOs is similar to that of MDs, encompassing four years of medical school. The curriculum includes traditional medical courses as well as additional training in the musculoskeletal system and OMT. DO students learn to consider the impact of lifestyle and environmental factors on a patient's health, fostering a comprehensive approach to care.
Like MDs, DOs must also pass a licensing examination known as the Comprehensive Osteopathic Medical Licensing Examination (COMLEX-USA). Upon completion, they enter residency programs, which are increasingly integrated with those of MDs, allowing for similar specialization opportunities. The osteopathic philosophy and the inclusion of OMT set DOs apart in their practice of medicine.
Historical Background of MD
The roots of allopathic medicine can be traced back to ancient Greece and the teachings of Hippocrates, who emphasized observation and diagnosis in medical practice. Over the centuries, medical science has evolved, leading to the establishment of formal medical schools and the adoption of evidence-based practices.
In the United States, the first MD degree was awarded in the late 18th century. The growth of allopathic medicine was bolstered by scientific advancements and the establishment of medical associations that standardized education and practice. This approach to medicine became the dominant paradigm, shaping modern healthcare systems.
The development of the MD degree reflects a commitment to scientific rigor and innovation. Advances in research, technology, and pharmacology have expanded the capabilities of MDs, enabling them to diagnose and treat a wide range of medical conditions with precision and efficacy.
Historical Background of DO
Osteopathic medicine was founded by Dr. Andrew Taylor Still in the late 19th century as an alternative to the prevailing medical practices of the time. Dr. Still believed in the body's natural ability to heal itself and emphasized the importance of the musculoskeletal system in maintaining health.
The first osteopathic medical school was established in Kirksville, Missouri, in 1892. The DO degree emerged as a response to the limitations of allopathic medicine, offering a more holistic approach that considered the patient's overall well-being. Dr. Still's philosophy laid the foundation for a distinct practice of medicine that incorporated hands-on techniques and a focus on preventive care.
Today, osteopathic medicine continues to grow in popularity, with DOs practicing in all areas of healthcare. The integration of OMT and the emphasis on treating the whole person remain central to the osteopathic philosophy, distinguishing DOs in the medical community.
Educational Path for MDs
The journey to becoming an MD begins with a bachelor's degree, typically in a science-related field. Aspiring MDs must complete prerequisite courses in biology, chemistry, physics, and mathematics. They then apply to medical school, where the competition is fierce, and acceptance rates vary by institution.
Medical school for MDs spans four years, divided into two phases. The preclinical phase includes classroom and laboratory instruction in subjects such as anatomy, physiology, biochemistry, and pharmacology. Students also learn about medical ethics, communication skills, and the social determinants of health.
The clinical phase involves rotations in various medical specialties, allowing students to apply their knowledge in real-world settings. These rotations cover areas such as internal medicine, surgery, pediatrics, psychiatry, and obstetrics and gynecology. During this time, students refine their diagnostic skills and gain exposure to diverse patient populations.
After completing medical school, MDs must pass the USMLE, a three-step examination that assesses their ability to apply medical knowledge and skills. Successful candidates enter residency programs, which provide specialized training in their chosen field. Residency can last between three to seven years, depending on the specialty. Upon completion, MDs may pursue further fellowship training or begin independent practice.
Educational Path for DOs
The path to becoming a DO is similar to that of an MD, starting with a bachelor's degree and completion of prerequisite courses in the sciences. DO applicants also undergo a competitive application process to enter osteopathic medical schools.
DO medical education consists of four years, with a curriculum that mirrors that of allopathic schools but includes additional training in osteopathic principles and practices. The first two years focus on classroom instruction in basic medical sciences, along with the introduction of OMT techniques.
In the clinical years, DO students participate in rotations across various specialties, gaining experience in diagnosing and treating patients. These rotations emphasize the integration of osteopathic principles, encouraging students to consider the patient's overall health and lifestyle factors.
DOs must pass the COMLEX-USA, a comprehensive licensing examination that evaluates their understanding of osteopathic medicine and clinical skills. Following medical school, DOs enter residency programs, which are now largely unified with MD programs, allowing for similar specialization opportunities. Residency training varies depending on the specialty, and DOs may pursue additional fellowship training post-residency.
Philosophical Differences in Practice
The philosophical differences between MDs and DOs are rooted in their respective approaches to patient care. MDs adhere to the allopathic model, which focuses on diagnosing and treating diseases through scientific methods. This approach emphasizes the use of medications, surgery, and other interventions to address specific health issues.
In contrast, DOs embrace a holistic approach, viewing the body as an integrated whole. They emphasize preventive care and the body's natural healing abilities, often incorporating OMT to improve musculoskeletal function and overall health. This philosophy encourages DOs to consider a patient's lifestyle, environment, and emotional well-being as part of their treatment plan.
While both MDs and DOs aim to provide high-quality care, their differing philosophies may influence their interactions with patients and the treatment plans they develop. The allopathic approach is often seen as more conventional, while the osteopathic approach offers an alternative perspective that prioritizes holistic health.
Clinical Approach of MDs
The clinical approach of MDs is characterized by a focus on evidence-based medicine and the application of scientific knowledge to diagnose and treat diseases. MDs are trained to identify symptoms and develop treatment plans that target specific health conditions using medications, surgery, and other interventions.
MDs often work in hospital settings, private practices, or specialized clinics, where they have access to advanced diagnostic tools and technologies. They collaborate with other healthcare professionals to deliver comprehensive care, ensuring that patients receive the most effective treatments available.
The allopathic model encourages MDs to stay up-to-date with the latest research and advancements in medical science, enabling them to provide cutting-edge care. This approach prioritizes precision and efficacy, making it well-suited for treating acute and complex medical conditions.
Clinical Approach of DOs
DOs employ a clinical approach that integrates osteopathic principles with traditional medical practices. Their focus on holistic care leads them to consider the patient's overall health, lifestyle, and environment when developing treatment plans. The use of OMT is a distinguishing feature of DO practice, allowing them to address musculoskeletal issues and enhance the body's natural healing processes.
DOs work in a variety of healthcare settings, including hospitals, private practices, and community clinics. They collaborate with other healthcare professionals to provide patient-centered care, often emphasizing preventive measures and lifestyle modifications to promote long-term health.
The osteopathic approach encourages DOs to view each patient as a unique individual, tailoring their care to meet specific needs. This perspective fosters strong patient-provider relationships and supports a comprehensive understanding of health and wellness.
Residency and Specialization Opportunities
Residency and specialization opportunities for MDs and DOs have become increasingly integrated, with both groups having access to a wide range of residency programs. This integration allows for similar career trajectories, enabling both MDs and DOs to pursue advanced training in various medical specialties.
MDs typically enter residency programs that align with their interests and career goals, such as internal medicine, surgery, pediatrics, or psychiatry. These programs provide intensive training and hands-on experience in the chosen specialty, preparing MDs for independent practice or further fellowship training.
DOs also have access to a diverse array of residency programs, thanks to the unification of accreditation systems. This integration allows DOs to train alongside MDs in specialties such as family medicine, emergency medicine, anesthesiology, and more. The inclusion of osteopathic principles in their training equips DOs with a unique perspective that can enhance their practice in various specialties.
The ability to specialize in a particular field of medicine offers both MDs and DOs the opportunity to develop expertise and advance their careers. Whether pursuing academic medicine, research, or clinical practice, the residency and specialization process is a critical step in shaping the future of healthcare professionals.
Career Opportunities for MDs
MDs have a wide range of career opportunities available to them, reflecting their extensive training and expertise in allopathic medicine. Many MDs choose to work in clinical settings, providing direct patient care in hospitals, private practices, or specialized clinics. Their focus on evidence-based medicine allows them to diagnose and treat a variety of health conditions, ranging from acute illnesses to chronic diseases.
In addition to clinical practice, MDs may pursue careers in academic medicine, conducting research and teaching future generations of healthcare professionals. Their background in scientific inquiry and medical knowledge positions them well for roles in medical education and research institutions.
MDs may also explore leadership positions within healthcare organizations, where they can influence policy and decision-making processes. Their expertise in patient care and healthcare management makes them valuable assets in administrative roles, contributing to the development of effective healthcare systems.
Overall, the career opportunities for MDs are diverse and varied, allowing them to tailor their professional paths to align with their interests and goals. Whether in clinical practice, academia, or administration, MDs play a vital role in advancing healthcare and improving patient outcomes.
Career Opportunities for DOs
DOs have numerous career opportunities that reflect their holistic approach to medicine and their expertise in osteopathic principles. Many DOs choose to work in clinical settings, providing patient-centered care in hospitals, private practices, or community clinics. Their focus on preventive care and holistic health allows them to address a wide range of medical issues while promoting overall wellness.
In addition to clinical practice, DOs may pursue careers in academic medicine, teaching and training the next generation of osteopathic physicians. Their emphasis on holistic care and OMT provides valuable insights for students and colleagues alike, contributing to the advancement of osteopathic medicine.
DOs may also consider leadership roles within healthcare organizations, where they can advocate for the integration of holistic approaches and osteopathic principles in healthcare delivery. Their unique perspective and expertise make them well-suited for positions that influence healthcare policy and practice.
The career opportunities for DOs are broad and varied, offering pathways in clinical practice, academia, leadership, and more. Their commitment to patient-centered care and holistic health positions them as valuable contributors to the healthcare community, enhancing patient outcomes and promoting wellness.
How Do Patients Perceive MDs and DOs?
Patient perception of MDs and DOs can vary based on individual experiences and understanding of each medical profession. Generally, patients may not be fully aware of the distinctions between MDs and DOs, as both are licensed physicians capable of providing comprehensive medical care.
MDs are often perceived as traditional medical doctors, with a focus on diagnosing and treating diseases using medications and surgery. Patients may seek MDs for their expertise in evidence-based medicine and their ability to address specific health concerns with precision and efficacy.
DOs, on the other hand, may be perceived as offering a more holistic approach to healthcare. Patients who value preventive care and the integration of lifestyle factors in treatment may be drawn to DOs for their focus on overall wellness and the use of OMT.
Ultimately, patient perception of MDs and DOs is influenced by individual preferences, healthcare needs, and prior experiences. Both MDs and DOs are dedicated to providing high-quality care, and patients may choose their healthcare providers based on personal beliefs and the type of care they wish to receive.
Can MDs and DOs Integrate Practices?
The integration of MD and DO practices is increasingly common in modern healthcare, reflecting the complementary strengths of both medical approaches. Many healthcare settings employ both MDs and DOs, allowing for a collaborative approach to patient care that combines the best of allopathic and osteopathic medicine.
MDs and DOs can work together to provide comprehensive care, leveraging their unique skills and expertise to address diverse healthcare needs. This integration fosters a multidisciplinary approach that enhances patient outcomes and supports a more holistic understanding of health and wellness.
In academic and clinical settings, MDs and DOs often collaborate on research, education, and patient care initiatives. Their combined efforts contribute to the advancement of medical knowledge and the development of innovative treatment strategies that benefit patients and healthcare systems alike.
The ability to integrate MD and DO practices reflects the evolving nature of healthcare, where collaboration and interdisciplinary teamwork are essential for delivering high-quality care. By working together, MDs and DOs can create a more inclusive and effective healthcare environment that prioritizes patient well-being.
What is the Key Difference Between MD and DO?
The key difference between MD and DO lies in their respective approaches to medical practice and philosophy of care. While both MDs and DOs are fully licensed physicians who provide comprehensive medical care, their training and focus differ in several significant ways.
MDs, or Doctors of Medicine, follow the allopathic approach to medicine, which emphasizes the diagnosis and treatment of diseases using scientific methods. Their training focuses on evidence-based practices, including the use of medications, surgery, and other interventions to address specific health issues.
DOs, or Doctors of Osteopathic Medicine, embrace a holistic approach to healthcare, viewing the body as an integrated whole. They receive additional training in osteopathic manipulative treatment (OMT), a hands-on technique that supports the body's natural healing processes. DOs emphasize preventive care and consider lifestyle and environmental factors in their treatment plans.
The distinction between MD and DO is not only philosophical but also practical, as it influences their clinical approach, patient interactions, and treatment methodologies. While both MDs and DOs aim to provide high-quality care, their unique perspectives contribute to a diverse and dynamic healthcare environment.
FAQs
1. Are MDs and DOs equally qualified to practice medicine?
Yes, both MDs and DOs are fully qualified and licensed to practice medicine. They undergo rigorous training and must pass licensing examinations to ensure they can provide high-quality medical care.
2. Do MDs and DOs work in the same healthcare settings?
Yes, MDs and DOs often work in the same healthcare settings, including hospitals, clinics, and private practices. They may collaborate to provide comprehensive care to patients.
3. Can DOs specialize in the same fields as MDs?
Yes, DOs can specialize in the same fields as MDs, thanks to the integration of residency programs. Both MDs and DOs have access to a wide range of specialties, including surgery, pediatrics, and internal medicine.
4. Is osteopathic manipulative treatment (OMT) used by all DOs?
While all DOs are trained in OMT, its use varies among practitioners. Some DOs incorporate OMT regularly in their practice, while others may use it selectively based on patient needs and preferences.
5. How can I choose between seeing an MD or a DO?
Choosing between an MD or a DO depends on your healthcare preferences and needs. If you value a holistic approach that considers lifestyle factors, you may prefer a DO. If you seek evidence-based treatment for specific conditions, an MD may be more suitable.
6. How does the integration of MD and DO practices benefit patients?
The integration of MD and DO practices offers patients a more comprehensive approach to healthcare, combining the strengths of both allopathic and osteopathic medicine. This collaboration enhances patient outcomes and supports a holistic understanding of health and wellness.
Conclusion
The difference between MD and DO is rooted in their respective philosophies and approaches to medical care. While both MDs and DOs are qualified physicians who provide comprehensive healthcare, their training and focus set them apart. MDs follow the allopathic model, emphasizing evidence-based medicine and the treatment of diseases through medications and surgery. DOs embrace a holistic approach, incorporating osteopathic principles and OMT to support the body's natural healing processes.
Understanding the distinctions between MD and DO is essential for patients, medical students, and healthcare professionals. By recognizing the unique contributions of each approach, individuals can make informed decisions about their healthcare providers and career paths. The integration of MD and DO practices in modern healthcare reflects the evolving landscape of medicine, where collaboration and interdisciplinary teamwork are key to delivering high-quality care.
As the healthcare industry continues to advance, the complementary strengths of MDs and DOs will play a vital role in shaping the future of patient care. Whether through clinical practice, research, or education, both MDs and DOs are committed to improving health outcomes and promoting wellness for all individuals.
You Might Also Like
Mastering Gutter Repair: Essential Tips For A Well-Maintained HomeMastering Signed Electronically Text In Letter Notice: A Comprehensive Guide
Unveiling The Nutritional Power: 1 Avocado Calories And Health Benefits
Wifi Modem Insights: A Comprehensive Guide To Connectivity
Misery Loves Company: The Intriguing Psychology Behind Shared Suffering
Article Recommendations
- Shirley Jones A Timeless Icon Of Film And Television
- Laura Wrights Children All You Need To Know
- Michael Jackson Through The Years A Legendary Journey